The impact of breathing on different HRV measurements: implications for monitoring athletes
Who, what & why?
It has long been known that breathing affects heart rate variability (HRV). Many studies have tracked HRV in athletes – some have used free (spontaneous) breathing, whilst some use controlled (paced) breathing, and they have all used a variety of different HRV measures, making comparisons between studies very difficult or even impossible.
The aim of this particular piece of work, performed by researchers at the Center for Research and Innovation in Sport in southern France was to compare daily variations in HRV using a variety of HRV measures in order to determine recommendations for practical use and future research.
This paper follows hot on the heels of work by leading researchers Plews, Buchheit et al. who made recommendations for practical HRV monitoring techniques, summarized here.
What did they do?
In a pilot study, they measured the free breathing rate of 10 male club runners in order to determine the most comfortable & natural rate at which to pace breathing in the main study.
They then performed two sets of waking measurements on each runner for a 3 week period, so that each subject performed both paced & free breathing every morning.
They analysed the data using a number of common HRV parameters, as well as resting heart rate (HR). They used both time domain (SDNN, RMSSD, SD1, SD2) and frequency domain measures (HF, LF, LF/HF, and total power TP).
The researchers looked at the amount of agreement (correlation) between the free & paced breathing data for each HRV parameter.
What did they find?
In the pilot study they found the mean freely chosen breathing rate to be 0.125 Hz (7.5 breaths / minute), which is about twice as slow as in sedentary people.
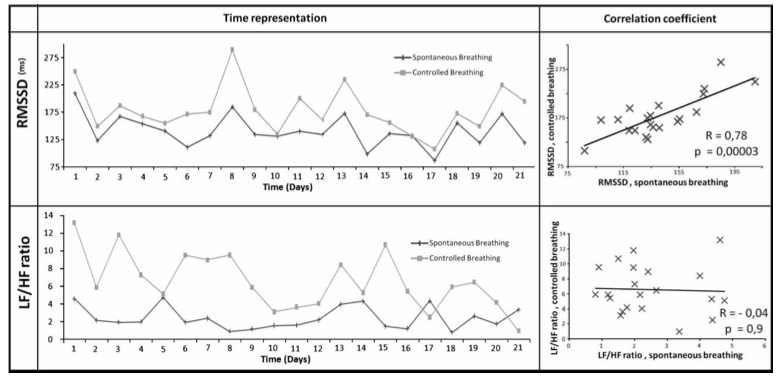
There were significant differences for all parameters between free and paced breathing, but out of all the parameters they looked at, only RMSSD and SD1 (SD1 is essentially the same calculation as RMSSD) showed a very significant correlation of 0.78.
A typical example from one of the athletes is shown below. You can see that the RMSSD, although at a different level, tracks well between the two breathing methods, whereas the frequency domain measure LF/HF ratio, often said to express ‘autonomic balance’, did not track at all, with zero correlation between the free and paced breathing measures. (We have previously explained why we don’t use this measure here: Why doesn’t ithlete measure low frequency (LF) power or LF/HF?)
What does it mean?
The naturally low free breathing frequency of athletes means that frequency domain HRV parameters are not suitable for longitudinal tracking of HRV over time. Making them suitable would involve paced breathing at rates much higher than athletes are comfortable with, which would in itself be stressful, thereby distorting HRV further.
The fact that the absolute values of HRV are different between the free and paced breathing cases is not significant when using monitoring apps like ithlete or Bioforce because all variations are compared to a moving average baseline. It’s also gratifying to see the breathing rate of 7.5 breaths / minute that we chose for ithlete nearly 4 years ago validated by the research.
As far as the choice of HRV parameters goes, the authors concluded that they “now prefer to use RMSSD or SD1 markers which are related to athletes’ fatigue (Kiviniemi et al., 2010; Plews et al., 2012) and provide the same variations whatever the breathing pattern” and “in agreement with recent works, we suggest using RMSSD or SD1 markers to perform relevant and reliable longitudinal HRV monitoring in order to prevent overtraining.”
To find the full paper:
The impact of breathing on HRV measurements: Implications for the longitudinal follow-up of athletes
Damien Saboul a b , Vincent Pialoux a & Christophe Hautier a


I am new to Myithlete and I have a query. When checking HRV why breathe in through nose and out through mouth? Is it correct that the optimum CO2 levels in our body have the effect of relaxing smooth muscle ( airway and blood vessels) and the best way to control this level is by breathing in and out through your nose. The risk being that if you breathe out through your mouth that you will wash too much CO2 out of the lungs resulting in a tightening of the airway.
Hi Ronan,
Its a good question. The idea when recommending this way of breathing was to provide a small inspiratory load to encourage slow breathing (which is good), and there is some evidence that nasal breathing may also stimulate the autonomic nervous system (ANS). We recommend breathing out through pursed lips to provide the load, though you could exhale through the nose if you prefer.
With respect to the CO2 levels, we consulted breathing expert Prof Alison McConnell, who says that there is a link between airway CO2 and airway smooth muscle contraction – hyperventilation (leading to hypocapnia) does induce airway smooth muscle contraction, so breathing slowly ensure this does not happen.