Introduction
During the early part of the pandemic, in June 2020, ithlete won a grant to try and determine whether or not changes in daily HRV could be used to detect the onset and subsequent severity of the illness. A summary of that study can be found here. What we didn’t know about at the time we conducted the survey of ithlete users, was how Covid would affect an otherwise healthy athlete’s ability to train during the illness and subsequent recovery.
Case study of a masters athlete infected in early 2020
We kept in contact with an ithlete user who had first got in touch in March 2020, and who suffered with symptoms that later became known as the Long Covid syndrome and which lasted for over a year.
The evidence was in their HRV. Their parasympathetic nervous system became increasingly disturbed, with their HRV dropping almost continuously for the first 3 months after catching Covid:
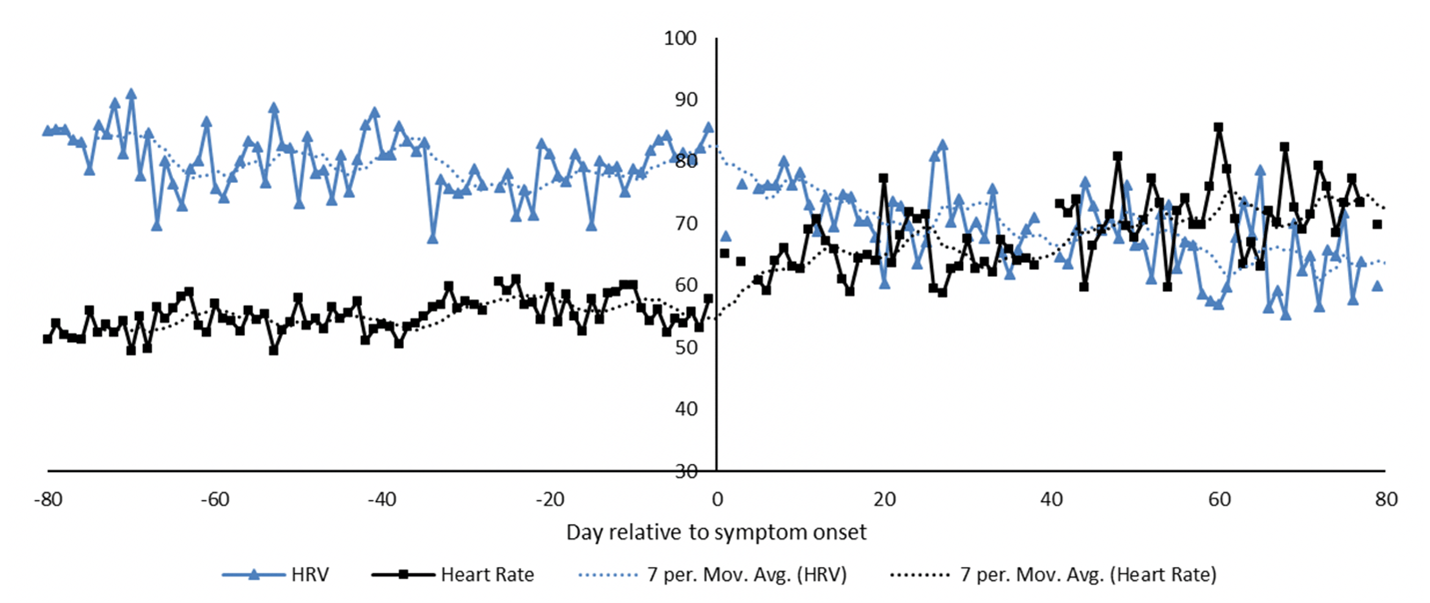
This ithlete user’s Heart Rate Variability (HRV) and resting heart rate was significantly disrupted for months after catching covid.
The chart also shows that their resting heart rate went from a nice steady value between 50-60 bpm to a spiky pattern that peaked at over 80 bpm on some mornings.
During this period, symptoms progressed from coughing, headache, nausea and shivering to breathlessness after even mild exercise, a metallic taste in the mouth, tingling in their fingers and poor-quality sleep.
The user’s symptoms were likely made worse by not only the lack of a vaccine but also the lack of any real knowledge in the medical community as to how to treat the condition, other than to regard it as a variant of chronic fatigue.
It was almost a year before they were able to return to frequent and moderately demanding bike rides.
Association between HRV and Covid severity
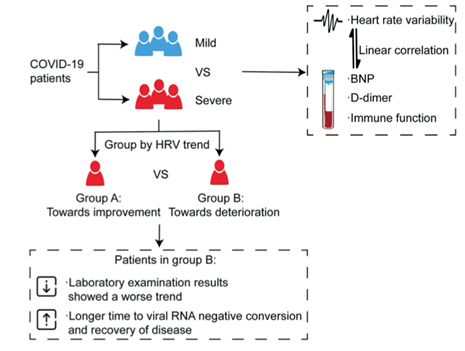
A study conducted on 34 patients with mild and severe Covid by the University of Wuhan in China published in May 2021 came to the conclusion that
‘HRV was associated with the severity of COVID-19. The changing trend of HRV was related to the prognosis, indicating that HRV measurements can be used as a non-invasive predictor for clinical outcome.’
For the study, patients were divided into a mild group (13) and a severe group (21). The severe group was further divided into two categories according to the trend of HRV (higher or lower over time). Severe patients had a significantly lower HRV (SDNN) than those with milder symptoms. D-dimer (a marker of blood clots), and NT-proBNP (a marker of potential heart muscle damage) showed a consistent trend with HRV in severe patients. The concentration of immune cells was lower in severe patients and those with lower HRV needed a longer time to clear the virus and recover.
HRV and Covid – a case study
More recently, in September 2021, a case study was published looking at the usefulness of using HRV for coaching athletes during and after viral infection.
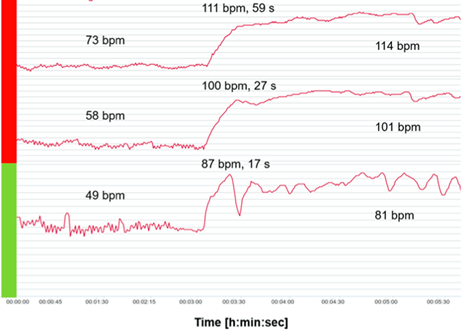
The athlete was a 30-year-old elite marathon runner who caught suspected Covid 4 weeks after competing in a marathon. They had intense flu symptoms and fever for 6 days, during which they (wisely) interrupted their normal training. What’s particularly interesting about this case study is that the athlete already had a good daily morning HRV measurement routine prior to becoming ill. They monitored their HRV (rmssd) and resting heart rate using a validated chest strap in both standing and supine (lying down) positions, and looked also at their peak HR response to standing:
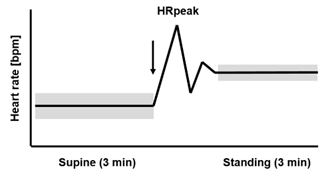
The arrow marks the change in body position from supine to standing up. The widths of the bars represent the higher HRV in the supine than the standing position.
The protocol used here is descended from the Rusko orthostatic stress & recovery test used with elite cross-country athletes in the late 1980s when HR monitors first became available (but long before the first HRV app, ithlete!). As can be seen in the chart, the change in heart rate from lying to standing gives the athlete an indication of how recovered they were, with a larger increase indicating a lack of recovery or impending sickness. The test was usually performed under supervision as it required calibration for the individual athlete to be interpreted usefully.
The charts below show how dramatically the Covid athlete’s resting HR increased in the first 2 days after becoming sick (red bar) vs the period before / after the acute sickness (green bar). Note also how much more variability there is in the HR trace during the green period, remembering variance is a good thing, showing the body is ready to respond to demands.
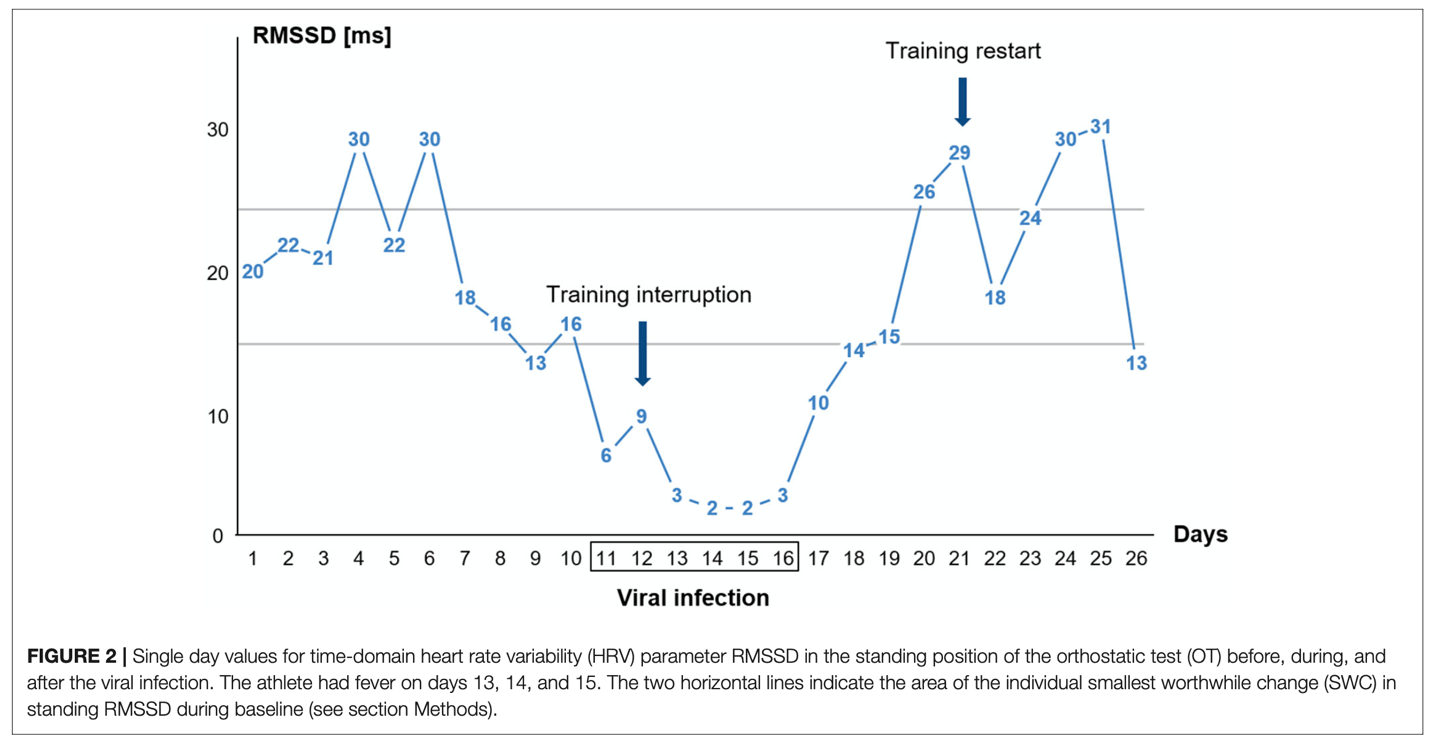
The chart below shows the athlete’s HRV for the entire period before, during and after the Covid infection. The HRV value at peak infection was 2ms (RMSSD) which is equivalent to an ithlete reading of 20 compared to their usual healthy HRV of 21ms (61 on the ithlete scale).
Conclusions
The authors of the case study concluded that the orthostatic test with a change from supine to standing body position and the detection of different indicators based on HR and a vagal driven time domain HRV parameter (RMSSD) is likely to be useful to detect viral diseases early on when implemented in a daily routine.
Evidence from the other athlete case and the study on patients in hospital confirms this view, and adds to reports we have heard many times over the years from ithlete users – that HRV is very sensitive to acute viral illnesses, often dropping precipitously shortly before they became sick.
The ithlete algorithms are designed to pick up not only acute drops in HRV which are tuned to the user but also the combination of an HRV drop and a rise in resting heart rate, which will give a red warning that is a sign to back off from anything potentially stressful until you see recovery in both metrics. These ithlete red indicators are rare, if you do get a red it is always worth considering the possibility that you are getting sick. You should restart training very cautiously once your HRV has improved and note the HRV response the next day, as your physiological reserve (or vagal tank as it’s sometimes known) is likely to be depleted for a while.
References:
- Pan Y, Yu Z, Yuan Y, Han J, Wang Z, Chen H, Wang S, Wang Z, Hu H, Zhou L, Lai Y, Zhou Z, Wang Y, Meng G, Yu L and Jiang H (2021) Alteration of Autonomic Nervous System Is Associated with Severity and Outcomes in Patients With COVID-19. Front. Physiol. 12:630038.
- Hottenrott Laura, Gronwald Thomas, Hottenrott Kuno, Wiewelhove Thimo, Ferrauti Alexander (2021). Utilizing Heart Rate Variability for Coaching Athletes During and After Viral Infection: A Case Report in an Elite Endurance Athlete Frontiers in Sports and Active Living VOLUME 3 2021
